The 2025 AHA and ILCOR resuscitation guidelines are here—and they’re stirring up debate. Dr. Sheldon Cheskes and Dr. Ian Drennan join Zach to break down mechanical CPR, vector change vs. DSD, epinephrine timing, airway choices, and what the evidence really says. A clear, honest deep-dive into cardiac arrest care.
Sponsored by:


Sheldon Cheskes
MD, CCFP (EM), FCFP
Dr. Sheldon Cheskes is a Professor with the Division of Emergency Medicine, Department of Family and Community Medicine at the University of Toronto, and a scientist at the Li Ka Shing Knowledge Institute at St. Michael’s Hospital in Toronto, Ontario, Canada. He is the Medical Director for the Regions of Halton and Peel with the Sunnybrook Centre for Prehospital Medicine. He is one of the principal investigators for the Canadian Resuscitation Outcomes Consortium (CanROC) and is a recognized international authority in the area of CPR quality and out-of-hospital cardiac arrest resuscitation. Dr. Cheskes has published over 100 manuscripts in high impact journals such as the New England Journal of Medicine, Circulation, CMAJ and Resuscitation that have changed resuscitation practice around the world.
He is the principal investigator of the DOuble Sequential External Defibrillation in Refractory Ventricular Fibrillation (DOSE VF) trial. This study will be the first cluster randomized trial to clinically evaluate two novel therapeutic defibrillation strategies (double sequential external defibrillation and vector change defibrillation) against standard practice for patients remaining in refractory ventricular fibrillation during out-of-hospital cardiac arrest. He is also studying methods to improve public access defibrillation in rural and remote areas through the use of community responder programs and drone delivery of automated external defibrillators.

Ian Drennan
ACP PhD
Dr. Drennan is a Paramedic Scientist, and an Assistant Professor in the Department of Family and Community Medicine (DFCM) and the Institute of Health Policy, Management and Evaluation (IHPME) and Associate Director of the Paramedicine Collaborative at DFCM at the University of Toronto. He is an Affiliate Scientist position at the Department of Emergency Services, Sunnybrook Health Sciences Centre and Affiliate Scientist, Li Ka Shing Knowledge Institute, Unity Health Toronto.
Dr. Drennan is the current vice-chair of the Advanced Life Support (ALS) Task Force for the International Liaison Committee on Resuscitation (ILCOR) and co-chair of the Basic Life Support chapter of the American Heart Association 2025 Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.
Dr. Drennan’s research interests are in the clinical care in the prehospital setting, including the management of life-threatening conditions such as cardiac arrest, stroke, STEMI, sepsis and trauma. Additionally, he has interests in alternative models of care and health system improvements for low-acuity patients from a prehospital / ED perspective.
Episode Overview
The highly anticipated 2025 AHA and ILCOR resuscitation guidelines have dropped—along with the expected debates and misunderstandings. In this packed episode, Zach sits down with two of the most influential voices in resuscitation science, Dr. Sheldon Cheskes and Dr. Ian Drennan, to walk through what the guidelines say, why they say it, and how clinicians should interpret them.
From mechanical CPR to epinephrine timing to double sequential defibrillation, this episode gives you the behind-the-scenes nuance straight from the people who helped shape the science.
Key Topics Covered
-
How Guidelines Are Actually Made
-
The structure of ILCOR, AHA, ERC, and national councils
-
Behind-the-scenes process: evidence reviews, consensus, and contentious votes
-
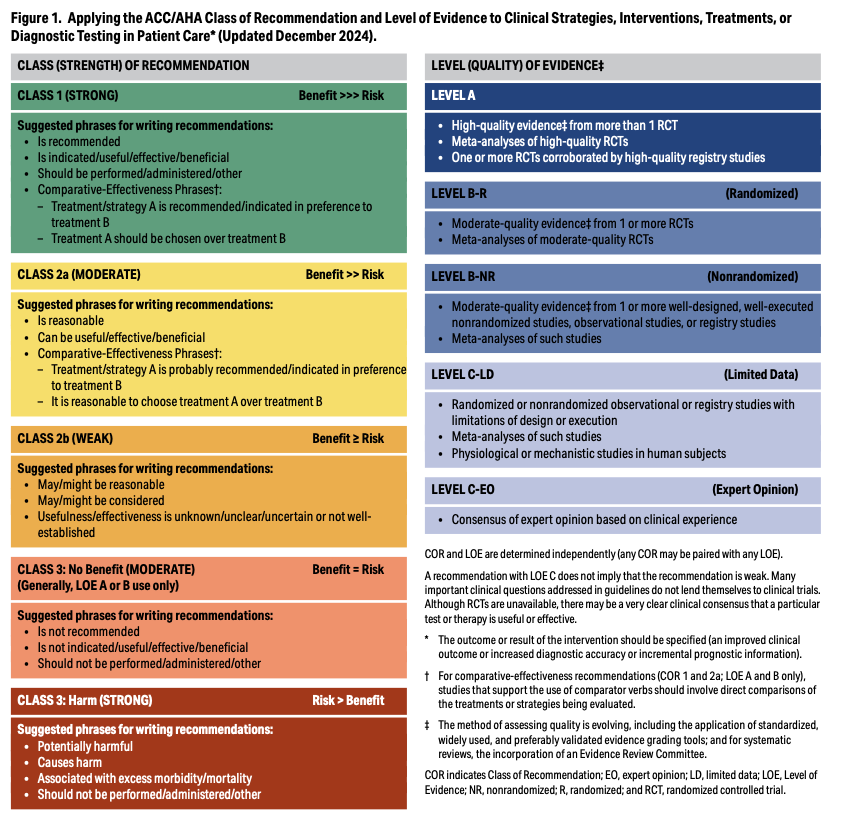
Why treatment recommendations have classes and levels of evidence—and what those really mean
-
Mechanical CPR
-
Still not recommended for routine use, but valuable in transport, limited personnel, hazardous scenes, and prolonged resuscitations
-
Emphasis on training, speed of deployment, and not delaying shocks
-
The guideline did not say “don’t use it”—and why that nuance matters
-
Heads-Up CPR
-
Physiologic appeal vs real-world limitations
-
Evidence remains animal-heavy and observational
-
Currently Class III – No Benefit
-
Vascular Access – IV vs IO
-
New large RCTs show no advantage of IO over IV
-
IO is not faster in real-world trials
-
Humeral IO frequently misplaced
-
Recommendation: Try IV first (Class I); move to IO if IV is unsuccessful (Class IIa)
-
Medications
Epinephrine:
-
Still Class I
-
Subtle change: now Class IIa for shockable rhythms
-
Debate on timing and dose—PITSTOP trial may shift practice
Other medications (calcium, magnesium, sodium bicarbonate, beta-blockers, naloxone):
-
Class III – No Benefit
-
No strong evidence for routine use
Amiodarone vs Lidocaine:
-
Still Class IIb
-
Important discussion on why we give them so late
-
Double Sequential Defibrillation (DSD) and Vector Change
-
Breakdown of the DoseVF trial results
-
Why DSD outperformed vector change
-
Misinterpretations in guideline wording
-
Problems with relying on “treatment received” analysis
-
Evidence from Sweden supporting early DSD
-
No documented harm; many systems continue to use DSD
Ian’s perspective:
-
How guideline committees balance new evidence
-
Why multiple confirmatory trials are sometimes required
-
Why this remains a Class IIb recommendation but is still supported in the right context
-
Airways and Ventilations
-
ETI should only be performed by clinicians with high first-pass success and ongoing training
-
SGAs are an excellent alternative for most systems
-
BVM alone is likely not reliable for prolonged care
-
Strong emphasis on ventilation quality and emerging feedback technology
-
Class III harm: Using ETCO2 cutoff values in non-intubated patients
-
Post–Cardiac Arrest Care
-
Avoid hypotension; target MAP ≥ 65
-
Avoid hypoxia and hyperoxia
-
Ontario context: dopamine should be retired; push-dose epinephrine likely coming; norepinephrine preferred
Practical Takeaways
-
Do not read guideline headings alone—read the supportive text and the strength of evidence.
-
New does not mean better, and “no benefit” does not mean “stop using it” in the right context.
-
Evidence-based practice is evolving, and this episode will help you stay ahead of the curve.





Recent Comments